References: 1. National Cancer Institute website. Accessed January 15, 2026.
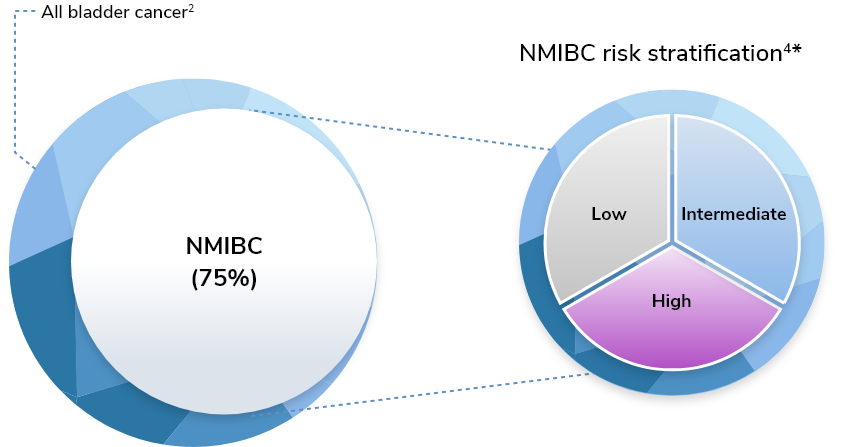
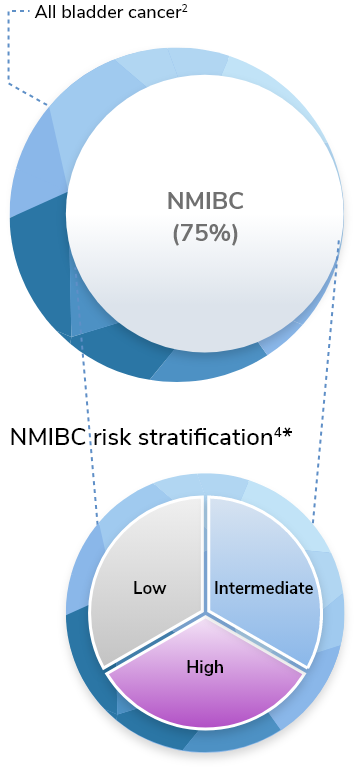
http://cancer.gov 2. Holzbeierlein JM, Bixler BR, Buckley DI, et al. Diagnosis and
treatment of non-muscle invasive bladder cancer: AUA/SUO guideline: 2024 amendment. J Urol. 2024;211:533-538.
3. Sylvester RJ, van der Meijden APM, Oosterlinck W, et al. Predicting recurrence and
progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined
analysis of 2596 patients from seven EORTC trials.
Eur Urol. 2006;49:466-477. 4. Holzbeierlein J, Bixler BR, Buckley DI, et al. Diagnosis
and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline: 2024 amendment. J Urol. 2024.
5. Soria F, Rosazza M, Livoti S, et al. Clinical validation of the intermediate-risk
non-muscle-invasive bladder cancer scoring system and substratification model proposed by the
International Bladder Cancer Group: a multicenter Young Academic Urologists Urothelial Working Group
collaboration. Eur Urol Oncol. 2024;7:1497-1503. 6. Ma J, Roumiguie M, Hayashi T, et
al. Long-term recurrence rates of low-risk non-muscle-invasive bladder cancer—how long is cystoscopic
surveillance necessary? Eur Urol. 2024;10:189-196. 7. Kukreja JB, Schroeck FR, Lotan Y,
et al. Discomfort and relieving factors among patients with bladder cancer undergoing office-based
cystoscopy. Urol Oncol. 2022;40:9e19-9e27. 8. Brisbane WG, Holt SK, Winters BR, et al.
Nonmuscle invasive bladder cancer influences physical health related quality of life and urinary
incontinence. Urology. 2019;125:146-153.
9. Cox E, Saramago P, Kelly J, et al. Effects of bladder cancer on UK healthcare costs
and patient health-related quality of life: evidence from the BOXIT trial. Clin Genitourinary Cancer.
2019;18(4):e418-e442. 10. Nayak A, Cresswell J, Mariappan P. Quality of life in
patients undergoing surveillance for non-muscle invasive bladder cancer—a systematic review. Transl
Androl Urol. 2021;10(6):2737-2749. 11. Casilla-Lennon MM, Choi SK, Deal AM, et al.
Financial toxicity in bladder cancer patients—reasons for delay in care and effect on quality of life. J
Urol. 2018;199(5):1166-1173. 12. Koo K, Zubkoff L, Sirovich BE, et al. The burden of
cystoscopic bladder cancer surveillance: anxiety, discomfort, and patient preferences for decision
making. Urology. 2017;108:122-128. 13. Griebsch I, Shrestha S, Lotan Y, et al. The
impact of intravesical instillations on quality of life in patients with non-muscle-invasive bladder
cancer: a systematic review. Oncol Ther. 2025;13:895-918. 14. Fink B, Son Y, Mueller T,
et al. The role of TURBT in bladder cancer: standardizing surgical approaches and future directions to
improve patient outcomes. Reviews in Urol. 2025;24:1-9. 15. Strother M, Barlotta R,
Uzzo R, et al. Symptomatic and functional recovery after transurethral resection of bladder tumor: data
from ecological momentary symptom assessment. Urol Oncol. 2024;42:117.e1-117.e10. 16.
Saint S, Trautner BW, Fowler KE. A multicenter study of patient-reported infectious and noninfectious
complications associated with indwelling urethral catheters. JAMA Intern Med. 2018;178(8):1078-1085.
17. Grabe-Heyne K, Henne C, Mariappan P, et al. Intermediate and high-risk
non-muscle-invasive bladder cancer: an overview of epidemiology, burden, and unmet needs. Front Oncol.
2023;13:1-17. 18. Parisse T, Reines K, Basak R, et al. Patient and provider perception
of transurethral resection of bladder tumor vs chemoablation for non-muscle-invasive bladder cancer
treatment. J Urol. 2023;209:150-160. 19. Nummi A, Jarvinen R, Sairanen J, et al. A
retrospective study on tolerability and complications of bacillus Calmette-Guérin (BCG) instillations
for non-muscle-invasive bladder cancer. Scandinavian J Urol. 2019;53(2-3):116-122. 20.
Alcorn J, Topping A. Withdrawing from treatment for bladder cancer: patient experiences of BCG
installations. Int J Urol Nursing. 2020;(3)14:106-114. 21. Maibom SL, Røder MA, Poulsen
AM, et al. Morbidity and days alive and out of hospital within 90 days following radical cystectomy for
bladder cancer.
Eur Urol. 2021;28:1-8. 22. Berger I, Leilei X, Wirtalla C, et al. 30-day readmission
after radical cystectomy: identifying targets for improvement using the phases of surgical care. Can
Urol Assoc J. 2019;13(7):E190-201. 23. Catto JWF, Downing A, Mason S, et al. Quality of
life after bladder cancer: a cross-sectional survey of patient-reported outcomes. Eur Urol.
2021;79:621-632. 24. Cerruto MA, D’Elia C, Cacciamani G, et al. Behavioural profile and
human adaptation of survivors after radical cystectomy and ileal conduit. Health Qual Life Outcomes.
2014;12:46. 25. Kamat A, Hafron J. Unmet needs in high-risk non-muscle-invasive bladder
cancer from the patient’s perspective: challenges and potential solutions. Rev Urol. 2024;23(4):29-39.
26. Inlexzo. Prescribing Information. Janssen Biotech, Inc.; September 2025.
27. Zusduri. Prescribing Information. UroGen Pharma, Inc.; June 2025.
28. Anktiva. Prescribing Information. Altor BioScience, LLC; April 2024.